Collaboration. Building on past experiences. Learning together.
These are the themes that come up consistently when you talk to the members of the Best Practice Spotlight Organization® (BPSO®) working group at East Toronto Health Partners (ETHP), the Ontario Health Team (OHT) serving East Toronto, about their efforts to embody the values of a BPSO OHT.
Joining the ranks of leading health-care organizations around the world, ETHP began the journey to become a BPSO OHT with the goals of improving patient outcomes through evidence-based practice and staff engagement. Three years in, the BPSO OHT has embarked on a number of initiatives to achieve the designation assigned by the Registered Nurses’ Association of Ontario (RNAO).
For Nursing Week, ETHP is celebrating the work achieved so far on our four-year BPSO OHT journey, which has come to life through the implementation of Best Practice Guidelines (BPG) that lay out specific practices for the OHT. With a commitment to Person- and Family-Centred Care and Preventing Falls and Reducing Injury from Falls, partners from across ETHP have come together to improve team-based care across organizations and promote learning within the OHT.
A tailored experience to learning about Best Practice Guidelines across the OHT

A screenshot of the Person- and Family-Centred Care iLearn homepage, developed by ETHP.
When it came time to educate team members on best practices in Person- and Family-Centred Care, leads from the BPSO Education group turned to their own experiences as BPSO designates before they joined the OHT.
Matt Wong, Manager of Professional Practice and Infection Prevention and Control Lead at VHA Home HealthCare (VHA), had helped implement the same BPG at VHA. Now, the task was to broaden that approach across the partnership.
“We thought: How do we take what we’ve learned and apply it to the BPSO OHT journey?”
One key learning from VHA was that a one-size-fits-all learning module wouldn’t be effective – providers had to see their unique experiences reflected in the module for it to be applicable to their work.
Wong and the team worked to ensure the module could be split off into different scenarios based on the role the learner selected. The result was a “choose-your-own-adventure” course that would apply the BPG work to each individual role. The partners at the table, including WoodGreen Community Services, South Riverdale Community Health Centre, and Michael Garron Hospital (MGH), came together to create scenarios reflective of roles across the OHT.
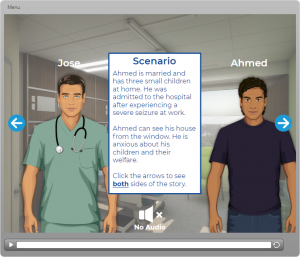
A screenshot of the Person- and Family-Centred Care iLearn scenario page, developed by ETHP.
“We recognized that we’re all used to developing something for our own context but we’re not going to work better together if we have a tunnel-vision approach,” Matt says.
The module the team created outlines a common understanding and framework around PFCC. It also orients frontline team members and managers to our vision and collaborative activities as ETHP. Stakeholders beyond the BPSO committee also reviewed the module. This included the engagement of ETHP client partners and community leaders from the training end.
“We hope that by engaging staff and teams across ETHP, the module will increase the satisfaction and enhance care experiences for clients and patients both as they’re brought on in their care journeys with the organizations of the OHT and as their healthcare needs change. By involving others to help review the scenarios presented in the learning for feedback, we hoped that it would help capture a variety of perspectives that individually may be missed due to implicit biases that influence a healthcare provider’s own personal worldview.”
Learning about the experiences of patients, caregivers and providers in an integrated care system
In 2021, ETHP was invited by RNAO to apply for support for a fellowship to evaluate the implementation of RNAO BPGs across an OHT. By working with mentors within the OHT, the Advanced Clinical Practice Fellowship aims to provide interdisciplinary health providers across the OHT dedicated time to develop knowledge and skills around BPG implementation.
Jennifer Reguindin, Clinical Resource Leader of Nursing Practice and Education at MGH, jumped at the chance to help others grow in their career.
“One of the things I’ve loved over my career is working with students and learners,” she says. “There’s a passion for building people’s careers and helping them reach their goals.”
Reguindin became the lead of the mentor group, and soon two fellows were selected: Kiel Ferguson, who was then a Registered Nurse in Critical Care at MGH, and Frances Montemurro, who was then a Pandemic Services Evaluator at South Riverdale Community Health Centre. The two fellows explored the experiences of patients, caregivers and staff as they transitioned between health sectors in ETHP as an example of the Person- and Family-Centred Care BPG in action. They focused their evaluation on the Primary and Community Care (PCC) Response Teams in East Toronto.

Pictured from left to right: Kiel Ferguson and Frances Montemurro, who were fellows in the Advanced Practice Clinical Fellowship, and Jennifer Reguindin, who led the mentorship group for the Fellowship.
The PCC Response Teams are an integrated care planning program offered by ETHP. They offer neighbourhood- and team-based health and social services care planning to help adults navigate the healthcare system, including those who may not have a family doctor, may be housebound and/or have unmet health or social needs by connecting them with additional supports and services that are close to home.
“This was a good opportunity to learn more about the community surrounding East Toronto,” Kiel explains.
The fellows performed a literature search and began data collection, pivoting with various waves of the pandemic. In the end, they developed a mixed methods approach of interviews and surveys. Their findings indicated that the neighbourhood and team-based model worked well overall and showed that care providers had created trusting relationships with clients.
“We try to do as much as we can for the people that we care for and I’m happy I got to see this integrated care system at the beginning,” Kiel says. “I’m excited to see how it grows.”
Jennifer and Kiel have been invited to present their work at a variety of events, including the RNAO’s International Advisory Council for NQuIRE. Now, the ETHP BPSO OHT is pursuing another fellowship for 2022 to continue the work Kiel, Frances, Jennifer and the mentor group began.
Adapting a tool to prevent falls and enable cross-provider collaboration
Falls are the leading cause of injury for older Canadians. According to Statistics Canada, with about one in four seniors experiencing one or more falls each year, they result in $2 billion a year in direct health-care costs.
As part of their BPSO OHT work, ETHP is implementing the Preventing Falls and Reducing Injury from Falls BPG, with the goal to enable and enhance falls prevention for clients across the partnership. Lori Sutton, Project Facilitator of Integrated Primary and Community Care at South Riverdale Community Health Centre, has been supporting a Champion Group that includes WoodGreen Community Services, Flemingdon Health Centre, and East End Community Health Centre to plan an approach for implementing this BPG.
“We did a gap analysis for falls prevention and found that having a common screening and assessment process and tool would be an important step,” Lori says.
Through their research, they found that the Centre for Effective Practice (CEP) had created a tool for primary care that was aligned with the Champions Group’s goals. Now, ETHP is working to adapt the tool so it can be applied across providers within organizations using Telus’s PS Suite electronic medical record with the hope for future spread to other organizations and platforms within the OHT
“The CEP tool is designed for primary care, where maybe one person would be filling out the screening and assessment form,” Lori says. “We’re working with CEP and a number of partners to adopt it for interprofessional use.”
The tool will be embedded in clients’ electronic medical records, and will prompt providers to fill it out for certain clients based on their risk factors.
“This way, we’ll have a proactive approach, with early identification and risk reduction,” Lori says. “We also hope the tool will help teams be aware of the individual’s risk of falls and collaborate with one another to reduce their risk.”
Although South Riverdale has been well-poised to lead this work with its strong focus on quality improvement and client and caregiver engagement, Lori says that the strength of existing relationships with organizations across the OHT has also been key.
“This work helps build our partnerships, but these aren’t new partnerships,” she says. “A tool like this can help build out the system that enables collaboration.”